‘Why? Why? Why?’ Ukraine’s Mariupol descends into despair
MARIUPOL, Ukraine (AP) — The bodies of the children all lie here, dumped into this narrow trench hastily dug into the frozen earth of Mariupol to the constant drumbeat of shelling.
There’s 18-month-old Kirill, whose shrapnel wound to the head proved too much for his little toddler’s body. There’s 16-year-old Iliya, whose legs were blown up in an explosion during a soccer game at a school field. There’s the girl no older than 6 who wore the pajamas with cartoon unicorns, among the first of Mariupol’s children to die from a Russian shell.
They are stacked together with dozens of others in this mass grave on the outskirts of the city. A man covered in a bright blue tarp, weighed down by stones at the crumbling curb. A woman wrapped in a red and gold bedsheet, her legs neatly bound at the ankles with a scrap of white fabric. Workers toss the bodies in as fast as they can, because the less time they spend in the open, the better their own chances of survival.
“The only thing (I want) is for this to be finished,” raged worker Volodymyr Bykovskyi, pulling crinkling black body bags from a truck. “Damn them all, those people who started this!”
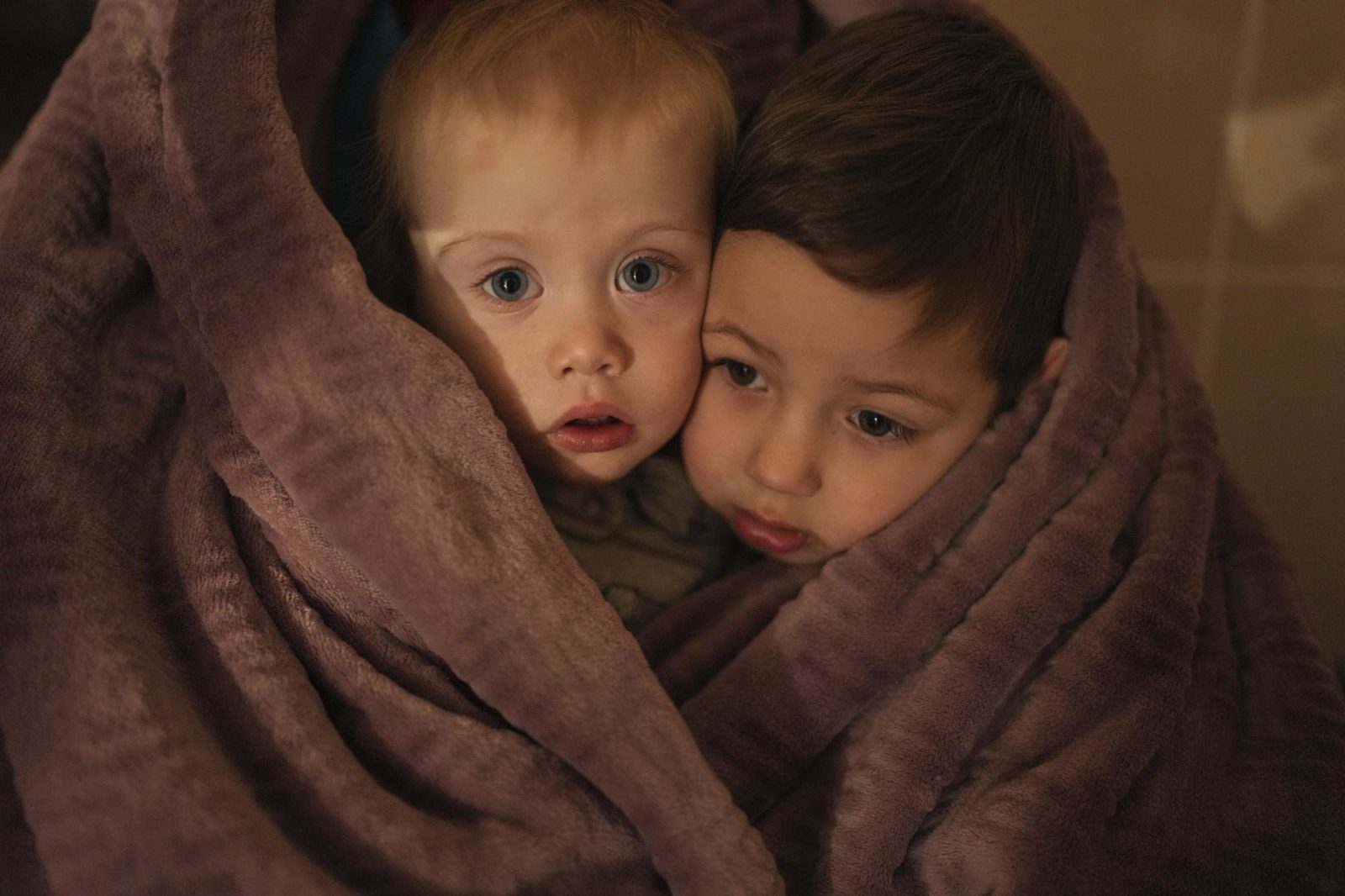
The children of medical workers warm themselves in a blanket as they wait for their relatives in a hospital in Mariupol, Ukraine, March 4, 2022. (AP Photo/Evgeniy Maloletka)

An apartment building explodes after a Russian army tank fires in Mariupol, Ukraine, Friday, March 11, 2022. (AP Photo/Evgeniy Maloletka)

A body lies covered by a tarp in the street in Mariupol, Ukraine, March 7, 2022. (AP Photo/Evgeniy Maloletka)
More bodies will come, from streets where they are everywhere and from the hospital basement where adults and children are laid out awaiting someone to pick them up. The youngest still has an umbilical stump attached.
Each airstrike and shell that relentlessly pounds Mariupol — about one a minute at times — drives home the curse of a geography that has put the city squarely in the path of Russia’s domination of Ukraine. This southern seaport of 430,000 has become a symbol of Russian President Vladimir Putin’s drive to crush democratic Ukraine — but also of a fierce resistance on the ground.
In the nearly three weeks since Russia’s war began, two Associated Press journalists have been the only international media present in Mariupol, chronicling its fall into chaos and despair. The city is now encircled by Russian soldiers, who are slowly squeezing the life out of it, one blast at a time.
Several appeals for humanitarian corridors to evacuate civilians went unheeded, until Ukrainian officials said Wednesday that about 30,000 people had fled in convoys of cars. Airstrikes and shells have hit the maternity hospital, the fire department, homes, a church, a field outside a school. For the estimated hundreds of thousands who remain, there is quite simply nowhere to go.
The surrounding roads are mined and the port blocked. Food is running out, and the Russians have stopped humanitarian attempts to bring it in. Electricity is mostly gone and water is sparse, with residents melting snow to drink. Some parents have even left their newborns at the hospital, perhaps hoping to give them a chance at life in the one place with decent electricity and water.
People burn scraps of furniture in makeshift grills to warm their hands in the freezing cold and cook what little food there still is. The grills themselves are built with the one thing in plentiful supply: bricks and shards of metal scattered in the streets from destroyed buildings.
Death is everywhere. Local officials have tallied more than 2,500 deaths in the siege, but many bodies can’t be counted because of the endless shelling. They have told families to leave their dead outside in the streets because it’s too dangerous to hold funerals.
Many of the deaths documented by the AP were of children and mothers, despite Russia’s claims that civilians haven’t been attacked.
“They have a clear order to hold Mariupol hostage, to mock it, to constantly bomb and shell it,” Ukrainian President Volodymyr Zelenskyy said on March 10.
Just weeks ago, Mariupol’s future seemed much brighter.
If geography drives a city’s destiny, Mariupol was on the path to success, with its thriving iron and steel plants, a deep-water port and high global demand for both. Even the dark weeks of 2014, when the city nearly fell to Russia-backed separatists in vicious street battles, were fading into memory.
And so the first few days of the invasion had a perverse familiarity for many residents. About 100,000 people left at that time while they still could, according to Serhiy Orlov, the deputy mayor. But most stayed put, figuring they could wait out whatever came next or eventually make their way west like so many others.
“I felt more fear in 2014, I don’t feel the same panic now,” Anna Efimova said as she shopped for supplies at a market on Feb. 24. “There is no panic. There’s nowhere to run, where can we run?”
That same day, a Ukrainian military radar and airfield were among the first targets of Russian artillery. Shelling and airstrikes could and did come at any moment, and people spent most of their time in shelters. Life was hardly normal, but it was livable.
By Feb. 27, that started to change, as an ambulance raced into a city hospital carrying a small motionless girl, not yet 6. Her brown hair was pulled back off her pale face with a rubber band, and her pajama pants were bloodied by Russian shelling.
Her wounded father came with her, his head bandaged. Her mother stood outside the ambulance, weeping.
As the doctors and nurses huddled around her, one gave her an injection. Another shocked her with a defibrillator. A doctor in blue scrubs, pumping oxygen into her, looked straight into the camera of an AP journalist allowed inside and cursed.
“Show this to Putin,” he stormed with expletive-laced fury. “The eyes of this child and crying doctors.”
They couldn’t save her. Doctors covered the tiny body with her pink striped jacket and gently closed her eyes. She now rests in the mass grave.

Oleksandr Konovalov, an ambulance paramedic, performs CPR on a girl injured by shelling in a residential area as her dad sits, left, after arriving at the city hospital of Mariupol, eastern Ukraine, Sunday, Feb. 27, 2022. The girl did not survive. (AP Photo/Evgeniy Maloletka)

The lifeless body of a girl killed during shelling at a residential area lies on a medical cart at the city hospital of Mariupol, eastern Ukraine, Sunday, Feb. 27, 2022. (AP Photo/Evgeniy Maloletka)
The same geography that for so long worked in Mariupol’s favor had turned against it. The city stands squarely between regions controlled by the Russia-backed separatists — about 10 kilometers (six miles) to the east at the closest point — and the Crimean Peninsula annexed by Russia in 2014. The capture of Mariupol would give the Russians a clear land corridor all the way through, controlling the Sea of Azov.
As February ended, the siege began. Ignoring the danger, or restless, or perhaps just feeling invincible as teenagers do, a group of boys met up a few days later, on March 2, to play soccer on a pitch outside a school.
A bomb exploded. The blast tore through Iliya’s legs.
The odds were against him, and increasingly against the city. The electricity went out yet again, as did most mobile networks. Without communications, medics had to guess which hospitals could still handle the wounded and which roads could still be navigated to reach them.
Iliya couldn’t be saved. His father, Serhii, dropped down, hugged his dead boy’s head and wailed out his grief.

Serhii, father of teenager Iliya, cries on his son’s lifeless body lying on a stretcher at a maternity hospital converted into a medical ward in Mariupol, Ukraine, March 2, 2022. (AP Photo/Evgeniy Maloletka)

Marina Yatsko, left, runs behind her boyfriend Fedor carrying her 18 month-old son Kirill who was fatally wounded in shelling, as they arrive at a hospital in Mariupol, Ukraine, Friday, March 4, 2022. (AP Photo/Evgeniy Maloletka)

Medical workers unsuccessfully try to save the life of Marina Yatsko’s 18 month-old son Kirill, who was fatally wounded by shelling, at a hospital in Mariupol, Ukraine, March 4, 2022. (AP Photo/Evgeniy Maloletka)

Marina Yatsko and her boyfriend Fedor comfort each other after her 18-month-old son Kirill was killed in shelling in a hospital in Mariupol, Ukraine, March 4, 2022. (AP Photo/Evgeniy Maloletka)
On March 4, it was yet another child in the emergency room — Kirill, the toddler struck in the head by shrapnel. His mother and stepfather bundled him in a blanket. They hoped for the best, and then endured the worst.
“Why? Why? Why?” his sobbing mother, Marina Yatsko, asked in the hospital hallway, as medical workers looked on helplessly. She tenderly unwrapped the blanket around her lifeless child to kiss him and inhale his scent one last time, her dark hair falling over him.
That was the day the darkness settled in for good — a blackout in both power and knowledge. Ukrainian television and radio were cut, and car stereos became the only link to the outside world. They played Russian news, describing a world that couldn’t be further from the reality in Mariupol.
As it sunk in that there was truly no escape, the mood of the city changed. It didn’t take long for grocery store shelves to empty. Mariupol’s residents cowered by night in underground shelters and emerged by day to grab what they could before scurrying underground again.

Serhiy Kralya, 41, looks at the camera after surgery at a hospital in Mariupol, eastern Ukraine on March 11, 2022. Kralya was injured during shelling by Russian forces. (AP Photo/Evgeniy Maloletka)

Medical workers treat a man wounded by shelling in a hospital in Mariupol, Ukraine, March 4, 2022. (AP Photo/Evgeniy Maloletka)
On March 6, in the way of desperate people everywhere, they turned on each other. On one street lined with darkened stores, people smashed windows, pried open metal shutters, grabbed what they could.
A man who had broken into a store found himself face to face with the furious shopkeeper, caught red-handed with a child’s rubber ball.
“You bastard, you stole that ball now. Put the ball back. Why did you even come here?” she demanded. Shame written on his face, he tossed the ball into a corner and fled.
Nearby, a soldier emerged from another looted store, on the verge of tears.
“People, please be united. … This is your home. Why are you smashing windows, why are you stealing from your shops?” he pleaded, his voice breaking.
Yet another attempt to negotiate an evacuation failed. A crowd formed at one of the roads leading away from the city, but a police officer blocked their path.
“Everything is mined, the ways out of town are being shelled,” he told them. “Trust me, I have family at home, and I am also worried about them. Unfortunately, the maximum security for all of us is to be inside the city, underground and in the shelters.”

People lie on the floor of a hospital during shelling by Russian forces in Mariupol, Ukraine, March 4, 2022. (AP Photo/Evgeniy Maloletka)

A Ukrainian serviceman guards his position in Mariupol, Ukraine, March 12, 2022.(AP Photo/Mstyslav Chernov)
And that’s where Goma Janna could be found that night, weeping beside an oil lamp that threw light but not enough heat to take the chill off the basement room. She wore a scarf and a cheery turquoise snowflake sweater as she roughly rubbed the tears from her face, one side at a time. Behind her, beyond the small halo of light, a small group of women and children crouched in the darkness, trembling at the explosions above.
“I want my home, I want my job. I’m so sad about people and about the city, the children,” she sobbed.
This agony fits in with Putin’s goals. The siege is a military tactic popularized in medieval times and designed to crush a population through starvation and violence, allowing an attacking force to spare its own soldiers the cost of entering a hostile city. Instead, civilians are the ones left to die, slowly and painfully.
Putin has refined the tactic during his years in power, first in the Chechen city of Grozny in 2000 and then in the Syrian city of Aleppo in 2016. He reduced both to ruins.
“It epitomizes Russian warfare, what we see now in terms of the siege,” said Mathieu Boulegue, a researcher for Chatham House’s Russia program.

People settle in a bomb shelter in Mariupol, Ukraine, March 6, 2022. (AP Photo/Evgeniy Maloletka)

A woman holds a baby in a bomb shelter in Mariupol, Ukraine, March 8, 2022. (AP Photo/Evgeniy Maloletka

People queue to receive hot food in a improvised bomb shelter in Mariupol, Ukraine, Monday, March 7, 2022. (AP Photo/Evgeniy Maloletka)

A man plays with a baby in a bomb shelter in Mariupol, Ukraine, March 6, 2022. (AP Photo/Evgeniy Maloletka
By March 9, the sound of Russian fighter jets in Mariupol was enough to send people screaming for cover — anything to avoid the airstrikes they knew would follow, even if they didn’t know where.
The jets rumbled across the sky, this time decimating the maternity hospital. They left a crater two stories deep in the courtyard.
Rescuers rushed a pregnant woman through the rubble and light snow as she stroked her bloodied belly, face blanched and head lolling listlessly to the side. Her baby was dying inside her, and she knew it, medics said.
“Kill me now!” she screamed, as they struggled to save her life at another hospital even closer to the front line.
The baby was born dead. A half-hour later, the mother died too. The doctors had no time to learn either of their names.

Ukrainian emergency employees and volunteers carry an injured pregnant woman from a maternity hospital damaged by shelling in Mariupol, Ukraine, Wednesday, March 9, 2022. The baby was born dead. Half an hour later, the mother died too. (AP Photo/Evgeniy Maloletka)

Mariana Vishegirskaya walks down stairs in a maternity hospital damaged by shelling in Mariupol, Ukraine, March 9, 2022. (AP Photo/Evgeniy Maloletka

Mariana Vishegirskaya lies in a hospital bed after giving birth to her daughter Veronika, in Mariupol, Ukraine, March 11, 2022. (AP Photo/Evgeniy Maloletka)
Another pregnant woman, Mariana Vishegirskaya, was waiting to give birth at the maternity hospital when the strike hit. Her brow and cheek bloodied, she clutched her belongings in a plastic bag and navigated the debris-strewn stairs in polka-dot pajamas. Outside the ruined hospital, she stared motionless with wide blue eyes at the crackling flames.
Vishegirskaya delivered her child the next day to the sound of shellfire. Baby Veronika drew her first breath on March 10.
The two women — one dead and one a mother — have since become the symbol of their blackened, burning hometown. Facing worldwide condemnation, Russian officials claimed that the maternity hospital had been taken over by far-right Ukrainian forces to use as a base and emptied of patients and nurses.
In two tweets, the Russian Embassy in London posted side-by-side images of AP photos with the word “FAKE” over them in red text. They claimed that the maternity hospital had long been out of operation, and that Vishegirskaya was an actress playing a role. Twitter has since removed the tweets, saying they violated its rules.
The AP reporters in Mariupol who documented the attack in video and photos saw nothing to indicate the hospital was used as anything other than a hospital. There is also nothing to suggest Vishegirskaya, a Ukrainian beauty blogger from Mariupol, was anything but a patient. Veronika’s birth attests to the pregnancy that her mother carefully documented on Instagram, including one post in which she is wearing the polka-dot pajamas.
Two days after Veronika was born, four Russian tanks emblazoned with the letter Z took up position near the hospital where she and her mother were recovering. An AP journalist was among a group of medical workers who came under sniper fire, with one hit in the hip.
The windows rattled, and the hallways were lined with people with nowhere else to go. Anastasia Erashova wept and trembled as she held a sleeping child. Shelling had just killed her other child as well as her brother’s child, and Erashova’s scalp was encrusted with blood.
“I don’t know where to run to,” she cried out, her anguish growing with every sob. “Who will bring back our children? Who?”
By early this week, Russian forces had seized control of the building entirely, trapping medics and patients inside and using it as a base, according to a doctor there and local officials.
Orlov, the deputy mayor, predicted worse is soon to come. Most of the city remains trapped.
“Our defenders will defend to the last bullet,” he said. “But people are dying without water and food, and I think in the next several days we will count hundreds and thousands of deaths.”

Anastasia Erashova cries as she hugs her child in a corridor of a hospital in Mariupol, Ukraine, March 11, 2022. (AP Photo/Evgeniy Maloletka)
Mykolaiv
Mykolaiv spreads out around the silver mirror of the Southern Bug River. The bridge over the Bug is raised, lowered, raised again. Every day, buses full of women and children depart for Odesa, which remains safe for now, though some flee farther still, to Moldova or to those parts of Ukraine not yet subsumed by war.
There are Russian divisions twelve miles to the north and east. They are shelling the outskirts of town.

Governor Vitaly Kim
Elena Kostyuchenko / Novaya Gazeta
Mykolaiv operates in blackout mode, no lights allowed after nightfall. The city administration has warned that a single individual’s failure to comply will result in the electricity being cut off for their whole building. Only the grocery stores and pharmacies remain open. Schools and day cares have been on break since the war began; no one wants to separate children from the adults. Many of the bus routes have been canceled; some of the buses have been requisitioned by the army and others deployed in the evacuation.
There are heaps of car tires sitting at the city’s intersections, ready to be ignited when Russian troops enter the city. Some still bear traces of paint from when they served as decorative borders for municipal flower beds. “One useful thing about the war,” said the mayor, “is that at least we’ll get rid of the rubber swans.”

Nikolaev
Elena Kostyuchenko / Novaya Gazeta
The lines for humanitarian aid packages are orderly: grains, tinned food, butter.
Everyday life takes place between air raids. The trauma center has been converted into a field hospital. Patients are evacuated as soon as their surgeries are completed and their wounds are patched up. Beds are then quickly cleared for incoming patients. The medical staff lives on-site and have done so for the past two weeks, since the war began.
Humanitarian aid comes through Odessa. The bigger city watches Mykolaiv with awe: Odessans believe that Mykolaiv is the only reason Odessa has not yet been besieged.
“Mykolaiv is partially surrounded,” says Yaroslav Chepurnoi, press officer for the Seventy-ninth Brigade. “There are seventeen Russian battalion tactical groups [BTGs] positioned around town,” he says. “Say each one consists of approximately a thousand men: that means seventeen thousand soldiers and fifteen hundred units of military tech—weapons, equipment, vehicles. We don’t know their command center’s plans, obviously; we can only assume that some of these BTGs will go north, possibly to Kryvyi Rih. But some of them will stay back and storm the city. We know that the Russian command has been ordered to take Mykolaiv, that it’s been ordered to take Odessa, and probably also to punch a land corridor to Pridnestrovie. So we are building up our defenses. Each day that goes by while they wait to attack Mykolaiv we use to build up our defenses.
“The Russian troops attacked a few times already. Four times, I think. The first three were just to gather intelligence. They came in small numbers, and we repelled them, blew up their vehicles. . . But March 7 was a proper attack, with rockets and tornado missiles at first, then they threw two BTGs at us.
“Here’s something interesting. They had plenty of weapons and carriers, but all it took for them to turn back and retreat was our blowing up a few tanks and a couple of armored vehicles. As soon as they took a bit of damage, insignificant damage, they turned around and retreated. We were surprised, frankly. When you launch an attack with tanks and armored vehicles, you expect to lose a few of them in the course of fighting. That shouldn’t prevent you from pushing on.
“According to the official count, there are three thousand captured soldiers across Ukraine. I trust those numbers. Even here, there are dozens and dozens. A couple days ago, we had twelve people surrender after some fighting. The fighting was over, even.
“They’re shelling the city with Grads and Hurricanes and Tornadoes. Grads may be only 122 millimeters, but Hurricanes are 240 millimeters and Tornadoes are 320: these are all multiple-rocket launchers. At first they targeted military installations. On February 24, they shelled our military airbase at Kulbakino, but our planes were already gone, so no dice. On the evening of the fourth, they targeted the railway station and the fuel storage tanks. Then the bread factory—I mean, God knows what they’re thinking. . . . And then, on the sixth and the seventh especially, they started heavily shelling the military units, as well as just residential areas. They’ve already hit the water treatment plants on the outskirts of the city a few times, so we figure they’re trying to mess up the water supply for the civilians. They’ve stationed artillery in the towns and villages between Mykolaiv and Kherson, that’s where they’re launching from.”
Shells rain down on Khersonskaya Street. This is Balabanovka, a residential neighborhood on the southernmost tip of the Korabelnyi district. The homes are so badly damaged they look half built. Slate tiles blown off the side of a fence, roofs sliding down into craters. The streets between the houses are strewn with the detritus of everyday life. A wall has shattered into bricks, though a little sign with the building number—22—survived. There’s no glass left in the windows, which makes the buildings look abandoned. A crumpled Gazelle van sits stowed behind a green gate.
Beyond the gate, a vegetable garden, the earth recently plowed. A cherry tree, strafed to the ground, its branches scattered across the warm earth. There are three gaping holes in the attic roof.

Consequences of shelling, Nikolaev
Elena Kostyuchenko / Novaya Gazeta

Sasha with a shell fragment in his hands
Elena Kostyuchenko / Novaya Gazeta
Sasha is up on a ladder, clearing the shattered slate tiles off the roof. He seems not to notice the tears running down his own face.
“First the shelling. A big whoosh over the wheat, all our windows blew out. Then it seemed to get quiet. My wife was on the porch, I was in the kitchen. She sits down. I take a look out the window and see these two airplanes from who knows where, black like the stealth ones. My wife fell over, and then rat-a-tat-tat! Some kind of white smoke. I threw myself over my wife and we started crawling. I’ve been picking up all the shards. Look how sharp they are, you can cut a person in half with that.”
His wife, Nadya, sits with her palms on her knees. “This is where I sat down. I was sitting right here. I’m sitting here, and there’s no sound at all. No sound for me to be afraid of. These two airplanes, they were scary, black or dark gray, but I didn’t even move from where I was sitting. I thought, ‘They’re not going to bomb civilians.’ And right at that second they started in on the ceiling. . . . I can’t tell you how terrifying it was. . . . Look at the gate, all the holes. Another moment, and that would have been me. I’m still in shock, I still can’t feel my legs. I’m terrified. Because the idea of leaving is terrifying, too. You still have to make it somewhere. This family I saw on the news, they were fleeing and they got caught in an air raid. The children died, and the parents, everyone.”

Nadia, Sasha’s wife
Elena Kostyuchenko / Novaya Gazeta
The Mykolaiv orphanage was evacuated immediately after the war began. There were ninety-three children living there, aged three to eighteen, all “social orphans,” children with living parents who cannot look after them. The children were taken to Antonovka, a village forty-one miles northwest. Five days ago, Russian troops assembled next to the village. On March 8, at 9:20 a.m., the troops fired on a car driving orphanage staff down the Kirovograd highway. Three women were killed.
Anatoly Geraschenko was the driver. He shifts anxiously from foot to foot. There’s a piece of shrapnel lodged in his right leg. “The surgeon said that they’ll operate if it starts to rot,” he says, but for now they’ve left it alone. Masha stays close to her father. One of her eyes is blue, the other one brown. “I’ve got three sons and two daughters,” Anatoly says proudly. He’s visibly shaking now, “It’s cold,” he says.
This was his third trip to Antonovka. He wouldn’t accept any money, only enough to cover the gas. He had stuck a red cross made of packing tape to his windshield. His van, a Mercedes Sprinter, burned along with the bodies inside.
“We made it past all the checkpoints, showing our passports every time. I had six women with me, and two in the back. At one of the checkpoints, they said something had gone down in the night. They shouldn’t have let us through!
“There was no oncoming traffic, just empty lanes. We made it about twenty-five kilometers. My vision’s not great, but two hundred and fifty meters out, the women spotted something, they tell me there’s something up ahead, something military. I said, ‘Ladies, what do we want to do?’ I slowed down. Then came the machine gun fire, I didn’t hear it or see anything. I only saw the gravel spraying out in front of me. Now I know why.
“I can’t remember exactly how they shot at us. Either I’d stopped completely by then, or maybe the van was still rolling a little. I didn’t see the blast, I only felt something shredding, dropping off of the van. A burst of light at my feet. I got out of the van, and they run over to me with their rifles. I’m lying facedown on the asphalt, screaming: ‘There are women inside! Women inside!’
“The Russians opened the back door—there were four more people in there. The women came out into the field. They ran over to them shouting, ‘Drop your phones!’ The women, four of them, all tossed their phones on the ground by the soldiers’ feet. I threw mine into the grass. I had a small one on me, in my pocket. My smartphone was still in the car, on the dashboard.
“When I go back to the van, it’s gone. I start looking for it. There was a woman sitting by the door—she had no face left. Just her guts out. Her finger was lying on the running board. Her face was gone! It was gone! And the woman sitting right behind me was dead, too, but her I didn’t see.

Burning car after shelling
Archive of Anatoly Gerashchenko
“The Russians are saying: ‘We warned you! We gave you a warning round.’ But I’m no soldier! Warning rounds aren’t the kind of thing I encounter every day. One of the women was wounded in the shoulder. They lifted her up onto her feet. One of the soldiers, a Yakut, or maybe he was a Buryat, bandaged her wound. The other one was very young, a kid, really. He had the same sunglasses as me. I remember his face. My leg was bleeding from all the shrapnel. This kid, he drew back when he saw me. Maybe he got scared or something. I said to him, ‘How do we get out of here?’ He says, ‘Take the fields. All the road signs have been taken down.’ I said, ‘We are going to walk on the road. If any of your men are up ahead, you tell them.’ They said, ‘We’ve informed them already.’
“They seemed completely indifferent, the Russians. They didn’t even care that the car was on fire, that there might still be people inside. I said to them, ‘Help me put it out, at least!’ They just stood there.
“I saw someone in the back lying there when the van first stared to burn. I got inside. It was this woman, her husband had seen her off, kissed her goodbye. I pulled her out—another woman helped me. We laid her out on the road and her back was all bare. I’d been dragging her by her jacket. Her back was shredded with shrapnel. I didn’t check her pulse or anything. Her husband called me today. I told him, ‘She didn’t burn, I pulled her out. . . . She’s still lying there.’
“There were two bodies left inside, they burned with the van. That car really burned. My birthday is November 11. And now it’s March 8, too.”
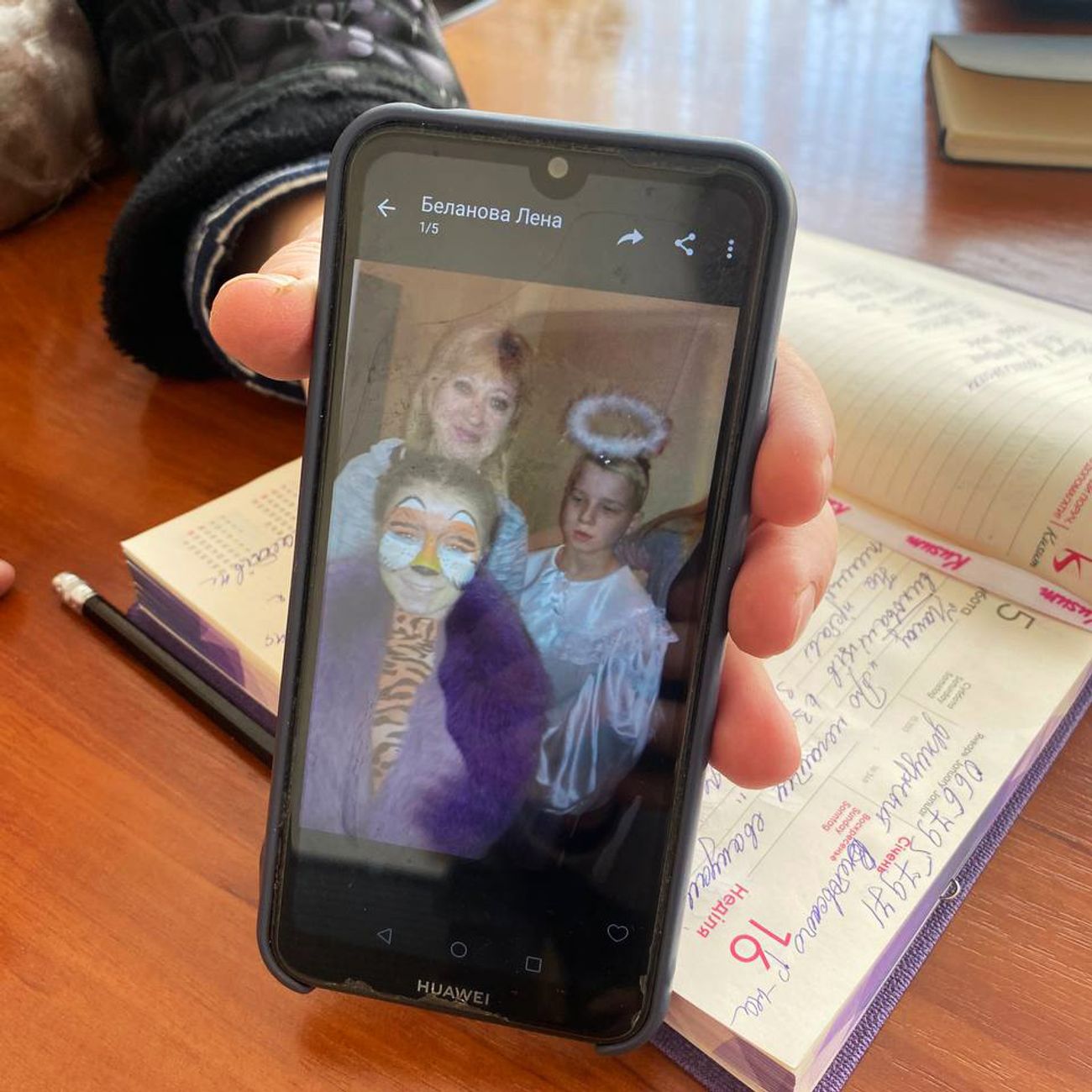
Principal Svetlana Klyuiko shows photos of the dead teachers. In the photo – Elena Alexandrovna Batygina
Elena Kostyuchenko / Novaya Gazeta
The three women killed were Natalia Mikhailova, Elena Batygina, and Valentina Vidyuschenko. The director of the orphanage, Svetlana Kluyko, tells me about each one of them: “Natalia Mikhailova, she’s been with us since 2014, a teacher. She used to work at a special-needs school so she was very experienced. She was the best sort of human being, kindness personified. If only there were more like her. She loved children, she was so wise, so good with her hands. All of my staff are excellent, but she in particular found a way to get on with everyone. She looked after the older boys. She would have been fifty on May 4. We were going to throw her a party. Elena Batygina took care of the little ones, dressing and changing them. Her children were always dressed so nicely. She had a big stock of different outfits, and party dresses. The children loved her, too. She was so kind. Twenty years with the orphanage. She was sixty-four. Valentina Vidyuschenko, she hadn’t been with us long. It was her second year as a teacher’s assistant. She was working with the new intakes, one of the most difficult groups. . . . When the children first come to us, they’re in tears. . . . They’ve been dropped off somewhere strange, it’s so stressful for them. She was one of the first people they met. She helped them wash, dressed them, changed them, talked to them, made them feel better. That’s the sort of people they killed. The children were inconsolable. They had been waiting for the teachers to come, we’d told them that they were on their way. The children screamed and screamed and wouldn’t stop.”
It was not possible to collect the bodies—or rather, what was left of the bodies: “We can’t get to them.” They remain where they were, fifteen and a half miles from the nearest Ukrainian checkpoint.
The wounded are in the Mykolaiv hospital: Anna Smetana, another teaching assistant, and Elena Belanova, a psychologist. The others, Galina Lytkina and Natalia Vedeneeva, have also been hospitalized, with “severe psychological trauma.”
Ninety-three children and ten teachers await evacuation farther into Ukraine in a village encircled by Russian troops.

Orderly in the mortuary bureau of forensic examination
Elena Kostyuchenko / Novaya Gazeta
All the dead pass through the office of the regional medical examiner. According to Olga Deryugina, its head, since the start of the war they have processed over sixty bodies of Ukrainian soldiers and more than thirty civilians. When I ask for the exact numbers, she replies: “What’s the point? New ones arrive every day.” Each body is examined by a team of investigators preparing to file documents with the International Criminal Court at the Hague.
“We’ve never had so many bodies at once. Shrapnel, bullet wounds, bomb blasts . . . shrapnel, mostly. We’ve had two corpses with unexploded munitions, the bomb-disposal technicians had to come out to defuse the bodies.”
“That’s right, there was an unexploded ordnance attached to the body, I removed it myself,” says Yuri Aleksandrovich Zolotarev, one of the medical examiners. “It hadn’t gone off because the fuse was damaged. I pulled out the casing to give to the bomb-disposal experts so that they could examine it. I told the women to stand back. . . . These had been soldiers. . . . I pulled it out very carefully and handed it over to the bomb-disposal technician. The fins were up inside the rib cage, but the fuse was inside the stomach—it hadn’t blown up because the stomach walls are too soft. That was when they were shelling Ochakovo—these were mostly bodies from there. . . . The other guy, it was only a part of an ordnance. When the women came to identify them, the wives, the way they wailed, I haven’t heard anything like that in my twenty years on the job. I was in the Bosnian war—I never saw such savagery. Two of our soldiers I autopsied—it wasn’t enough that they finished them off with bullets, they also had to knife them in the back. . . . On March 6, two young guys went over to the aircraft repair facility, to try to torch it with Molotov cocktails. . . . The soldiers caught them, tied them up, shot them in the head, and then finished them off by stabbing them in the back. They had knife wounds, dagger wounds under the shoulder blade. It’s barbaric, taking the wounded and finishing them off like that.”
“First they shot them and then they finished them off?”
“I’ve been a medical examiner for twenty years! I know which of those wounds came first.”
The bodies are piled up in two sections of the cold storage. But there isn’t enough room in there, so the ones that have already been autopsied are stacked outside in the street, beside the wall. Eight of them, in black body bags. An outbuilding that was used as a shed before the war is now full of bodies, too—two rooms, each of them sixty-five feet across. There are bodies all over the floor. Five Russian soldiers lie in a corner. “We’re keeping them while it’s cold outside. Nobody knows who we should hand them over to, or how.
“These are all war fatalities, the burn victims are already body-bagged. . . . Step over them, don’t be scared. I’ve got some others here, too. Once we’ve worked them over, we have to pack them up in these black plastic bags, because, to be honest, there’s nowhere to put all the autopsied bodies, you’ve seen the state of the rooms.”
There are bare feet and feet still wearing shoes. Here is a scorched, blackened young man on his back, arms spread wide, a charred black mess for a face. Half of a human body, flesh fused with grass, a jacket covering the head, and a man’s hand hanging down from under the jacket. A naked man wrapped in a floral sheet. A Russian soldier with his hands behind his head; his camo jacket is riding up and you can see a clean undershirt and the yellow strip of his belly.
The bodies in the cold storage are stacked up in layers. Two girls lie one on top of the other. They are sisters. The older one is seventeen. All I can see in the heap of bodies is her hand, her slim, long fingers with neat pink nail polish. The younger girl is three years old and lies on top of her sister. She is blond. Her jaw has been tied shut with gauze, her hands tied together to rest on her stomach. Little red wounds from the shrapnel cover her body. The girl looks alive.
Arina Butym and Veronica Birykova. Same mother, different fathers. They came in on March 5, at five p.m. They’re from the Meshkovo-Pogorelovo village, Shevchenko Street.” Nikolai Chan-Chu-Mila is an orderly here. He doesn’t look at me when he speaks. “I’m their godfather. . . . I did their baptisms. We’re old friends. They brought the girls in during my shift. Of course I recognized them straightaway. I can’t describe what I went through when I first saw them.”
Dmitry Butym is the girls’ father. He waits on the other side of the fence, he’s taking their bodies home today. Deep red folds rim his eyes. “Vera was heating up food in the kitchen. Arina had gone out to play in the yard. They didn’t have a chance, either of them. The little one died instantly, a piece of shrapnel through the heart. The older one, they got her heart going for two minutes, but it wouldn’t beat on it own. Their mother is in the Dubki hospital, she has shrapnel in her thigh—it damaged things as it went through. You have to excuse me, all I can think about right now is burying my children.”
There’s a new body being brought in. The attendants are unwinding a striped bedsheet. It’s a man, the breathing tube still in his throat and his body flayed. Somebody tried to save him but couldn’t. He is left to lie in the yard.
Four men with dark roses are waiting for their colleague to be released to them. Igor was a security guard, a civilian. “That goddamn Tornado comes down, and that’s it.”

Elena Kostyuchenko / Novaya Gazeta
A body in camo trousers is carried out from the shed. The body is purple, with a wide gash where a face should be. Two men from the investigations unit bend over him. They take down a description of his clothes, remove his trousers, take a DNA sample by dipping a piece of gauze in his blood. One of them pokes his fingers into the crushed mess of the man’s mouth—they need to establish which of the skull bones are broken.
A light-haired woman wrapped in a black headscarf speaks: “My mother lived on the fifth floor. She couldn’t get down to the bomb shelter in the cellar. Her next door neighbors, they helped her, they were like family. She died in the morning, peacefully. As much as you can call it peaceful—she was on the bathroom floor, hiding from all this horror. The next day, at exactly the same time, a rocket hit the building next door and blew out all of her windows. But she was already gone by then. I think it was some kind of miracle, that she died peacefully on the Sunday. The next day she would have died in a state of terror. She was seventy-seven. I have a photo of the apartment, what was left of it, from the neighbors. This is the view from her window, the building next door that was hit. It was the next day, she wouldn’t have survived it. She died on Forgiveness Sunday. And on the seventh all of her windows burst. She would have been so frightened. If it had to happen, I’m glad it was on the sixth and not on the seventh. I’m so grateful. My mother was named Svetlana Nikolayevna. She was half Russian. Her husband, my dad, was born in Russia, in Krasnoyarsk. He was stationed here, that’s how they met. My maternal grandfather was from Kursk. We were a Russian-speaking family. We’re going to the cemetery now. My son is in Kyiv. My name is Oksana.”

Barracks of military unit A0224 after shelling
Elena Kostyuchenko / Novaya Gazeta
Army base A0224 is one of the two military installations at Mykolaiv that was hit by artillery fire. On March 7, at 5:15 a.m., the barracks were struck by a Caliber rocket. Nine dead, including five conscripts who had not yet seen fighting. Fourteen wounded. Two of the conscripts initially presumed missing in action were found several hours later—they had fled and hidden.
A chunk of a three-story building has been reduced to rubble. There’s a bunk bed still sitting on an intact bit of floor. Emergency responders dig through the rubble by hand. They work with the military personnel, passing the pieces up a human chain. They are searching for the body of the last missing man. His name was Stas. He was a native of Western Ukraine and had been drafted eight months ago.
Yaroslav, the press officer, had a lucky escape that night. He is squinting at the sun, his hands never not on his rifle. “They sounded the alarm at about five fifteen. I shot up and shouted, ‘Boys, everyone out!’ We were the first ones out of the barracks, we didn’t even put our boots on. . . . There were guys standing outside, and I told them to get inside. God forbid that they hit us with something, the shrapnel would go everywhere. . . . I started to go back inside. I ran back in and when I got to the second floor, maybe seven meters from me, I saw the tiles flying up, then a flash—fire. I saw fire. At five seventeen they hit us.
“I was knocked back by the blast. I covered my head with my arms. There was glass raining down on me. I try to turn on my . . . Fifteen seconds pass and I turn my flashlight on and I’m crawling. I can hear people screaming, a woman was screaming. I’m crawling and crawling, but I can’t feel the ground under me anymore. There is no ground. I hear the sergeant shouting, ‘Everybody outside!’ I managed to get back and started to run out. I had my rifle with me. Everybody I saw, whoever was left, I told them: ‘We have to get down to the shelter.’ And that’s how we made it out. Taras, Danila, some of the other guys, they were all buried under the rubble. There had been twenty-nine of us in the sleeping quarters.
“I don’t want to start cursing . . . but I’m not taking prisoners, not after this. And I don’t care about their parents or wives. I don’t feel any pity. I’m twenty years old, I was training to be a veterinarian, but I don’t have any pity left for anyone.”

Anthony and Yaroslav
Elena Kostyuchenko / Novaya Gazeta
Somewhere up at the front lines, the Ukrainians have shot up a Tiger infantry mobility vehicle. Its Russian crew of four has surrendered. At HQ, they think that the Russians were doing reconnaissance, but those who were actually there think the Tiger was probably just lost.
Arthur has a black bandanna over his face. In his former life, he was a specialist in economic cybernetics. “There was a car driving up from the direction of Kherson. When it got here, I saw it was armored. They rolled down a window. I look inside: Russians, in uniform. I say, ‘Surrender.’ I cursed at them, too. The guy rolls the window back up before I could shoot. I started shooting out their tires. The car rolled for maybe another twenty seconds. Somebody threw a grenade and the car burst into flames. They didn’t want to come out at first. We smashed the windows in, and then they began to surrender.”
“Did you talk to them?”
“We tried not to. These terrifying warriors. All our guys were laughing their asses off. It was the usual bullshit: they thought that they were just doing military exercises, all of that crap. ‘I don’t even know where I am.’ Total bullshit, of course they know.”
They handed the prisoners over to the Security Service.
Someone has graffitied “Death to the enemies” on the dividing line in the middle of the road. The soldiers are warming up by the wood-burning stove. “Those Russians fucked up our spring.”
“I heard that it came from those towers,” says a soldier nicknamed the Actor. “A sniper or a machine gunner, I don’t know for sure. One bullet hit forty centimeters from my foot. After the third bullet, I finally clocked that they were aiming right at me.”
“Are you waiting for them to storm the city?”
“I’m waiting for all this fuckery to fuck back off. And I hope that the residents of the occupied territories are making plenty of Molotov cocktails. And I’d like to wish my daughter happiness. She’s three. I named her Maria.”
“My family stayed. My brother’s house is a little bigger than mine. We all live in the same village—my brother, our mother, and me. My brother is older, so he’s the head of the family, you know how it goes. His job is protecting the women and children, my job is to be here. I was in Varvarovka when they shelled the Kulbakino air base, working at a shipbuilding plant. My uncle woke me up at six thirty, and we could hear the air base being shelled. I was at the central recruiting office by eight twenty. They gave me my enlistment papers and said to come back at six o’clock the next morning, all packed. I only told my wife after I got back. She knew, though—she knew I would do that.”
“Where could we evacuate to? This is our land,” says another soldier. “My family is in Odessa. They won’t touch Odessa while Mykolaiv is standing. That’s why I’m here.”

Ukrainian military
Elena Kostyuchenko / Novaya Gazeta
“We keep saying: ‘Russians, go home! Just go home, that’s it. We didn’t ask you to come here. You don’t have to die here.’”
“Why won’t they collect their corpses? They’re just fertilizer for our fields. So sorry, but your son will come here and you’ll never see him again, no neat little grave for you to visit. Something happens to me, though, my mom will grieve for me and bury me herself.”
“People who used to be like brothers to us are our enemies now, because they attacked us—that’s not what brothers do. We have to defend our land, we have to stand our ground. We didn’t want this war, we didn’t see it coming.”
“I’m from Mykolaiv myself. Am I supposed to just sit home and wait? I went down to the recruitment office on the very first day.”
“We don’t want to wage war against Russia. So don’t you come and wage war against us.”
“They think Ukraine is weak. No. Ukraine is really good. We know every hole and every burrow here. This is our land you’ve come to.”
“We don’t want war. We want you to leave us alone.”

Maternity room in the basement of maternity hospital No. 3
Elena Kostyuchenko / Novaya Gazeta
So far, twenty-two babies have been born at the Mykolaiv maternity hospital No. 3 during the war, two of them in the makeshift bomb shelter in the basement. All of the babies survived.
There are almost no C-sections anymore, because the stitches need rest, peace, and quiet, and there’s no peace now, not with the air raids. A maternity ward has been set up in the basement, but the operating rooms are still on the third floors. This is very dangerous. A siren blares. Expectant mothers walk down to the basement, step by step, holding on to the walls, their descent slow and ponderous. The midwives carry the babies down.
Lena Sylvestrova lies on a metal gurney under a woolen blanket. Her husband, Aleksei, is trying to soothe her. The palm of his hand is on her neck. Lena gave birth at 4:30 a.m. by C-section. She had tried for a natural birth, she labored for almost twenty-four hours. She is twenty-eight and her husband is twenty-six. This is their first child. She went into labor early in the morning, after curfew. Aleksei drove her to the hospital himself.
“My due date was just around when the war started. I was so worried, waiting for it all to kick off. I was constantly on edge, waiting. Worrying that we’d get caught in an air raid or shelling in town. I was lucky—they managed to do my C-section between two air raid sirens. Imagine, you are in labor, all you want is some peace and quiet for your baby, but instead, your city is being endlessly bombed!”

Alexey and Lena, a young mother
Elena Kostyuchenko / Novaya Gazeta
Aleksei strokes her cheek.
“I’d love to remember what it’s like, walking around without worrying about getting shot.”
The light in the basement is dim, the women sit along the walls. The chief physician takes Aleksei to the archive department and quietly opens the door. Inside, a midwife sits on some mattresses and cradling a white bundle. She holds the bundle out toward Aleksei. “I don’t want to hold it, I’m scared,” he tells her.
“Better get used to it. Don’t be scared, nothing to be afraid of.”
Aleksei holds Masha in his arms. It’s his first time. The midwife gently adjusts his hands.
“She’s so tiny,” Aleksei says. He falls silent, his face dipping ever closer to his daughter’s. “My little girl. Hello there! Are you sticking your tongue out at me? Really, Masha? We’re going to be together every day, every single day, deal?”

Alexey and newborn Masha
Elena Kostyuchenko / Novaya Gazeta
We only want peace. Please write that,” says a woman in a white lab coat. “My name is Nadezhda Sherstova. I’m a senior nurse anesthetist. I’ve been doing this job thirty years. Since the war started, whenever a baby is born, there’s no joy in the parents’ eyes. You worry about the mothers, their milk coming in. That’s what scares me. There is no joy for the parents.”
“She was a real pain,” Aleksei tells the chief physician. “Constantly kicking. She’d hear my voice and start in on her dancing in there. Wouldn’t let her mom sleep at night. She’s kicking a little right now. I thought she would look like me. When we did the ultrasound, they said she looked like me, but look how pretty she is.”
The next shelling of Mykolaiv began at 8:00 p.m. on March 11 and lasted most of the night, with brief pauses. According to Mayor Oleksandr Senkievich’s official statement, more than 167 residential buildings sustained damage, including City Hospital No. 3 (which was filled with wounded civilians), a prepared-food plant, eleven schools and day cares, and an orphanage. Eleven private homes were completely destroyed. Shrapnel shredded the yard of the cancer ward and the emergency department. Kuzya, the beloved hospital guard dog, was killed. They covered him up with a towel. The cemetery was shelled, too. Fires have broken out all over the city.

