3,000 Nautical Miles of Hope
The sea was calm and smooth off the Brazilian coast on the morning of 10 July when a police patrol boat approached the grain freighter Ken Wave, eight nautical miles from the city of Vitória. The authorities had been alerted after the crew of the Nigerian-registered freighter spotted a group of stowaways.
One of the officers raised his smartphone, zooming in on the massive, rust-coloured hull. There, perched on the rudder blade, were a few tiny figures—crouched, exhausted, as if they had just been spat out by a whale, like Jonah.
“Sir, do you speak English?” shouted the Brazilian. “How many people?”
“Four!” shouted one of the men, who was wearing a tattered denim shirt.
“Do you have food or water?”
The men responded with gestures that vehemently denied this. “Okay, we’re here to help you,” the police officer called out, then he explained that they were now fetching life jackets, water, and some chocolate. This was the last scene of the video sequence that would soon spread across the world—the final stage of a 14-day odyssey had narrowly avoided ending in death.
If the Ken Wave, which was on its way to Santos, hadn’t briefly anchored off Vitória to take on a new crew, any help would likely have come too late for Thankgod Yeye, Roman Friday, Sunday Ugbo, and Destiny Eze.
And so, after spending a night in the soft beds of a hotel, the four Africans sat before a migration officer, trying to put into words what on earth had led them to attempt crossing the Atlantic in the cramped, stifling shaft housing a cargo ship’s steering column.
Their statements were sparse, consisting of brief sentences that boiled down to economic hardship. They spoke of having no work, no home, and no future in their homeland. “Nigeria is hell,” Roman said, explaining that he had pinned all his hopes on Europe. What they hadn’t realized was that the ship was heading southwest, each cursed day carrying them farther from their destination.
But—did that truly explain anything?
According to the International Organisation for Migration, there are more than 280 million displaced people worldwide. They flee wars, conflicts, political persecution, droughts, floods—or simply the grinding poverty of a country like Nigeria, where half the population dreams of a life elsewhere.
Their problem is that they are increasingly being perceived as a threat in the prosperous countries of Europe and North America. To appease their citizens, governments are fortifying borders, making them ever harder to cross. Europe is pouring millions into the coast guards of North African transit countries and seeking third-party states to process asylum applications on African soil. Repatriation agreements aim to expedite deportations of those who are turned away.
The doors are rarely opened anymore.
To address labor shortages, Germany is now actively seeking skilled workers from West Africa. But this is a kind of cherry-picking policy targeting those who already have good career prospects at home. For the vast majority, like Thankgod or Roman, the cost of a visa alone is an impossible to afford, so legal migration is an illusion.
As a result, for an ever-growing number of people, the routes are becoming ever more complex—and far more dangerous. By 1 June, 200 Nigerians had already drowned in the Mediterranean or perished crossing the Sahara. In April, a stowaway froze to death in the landing gear of a KLM plane flying from Lagos to the Netherlands. In September 2022, the crew of a Panamanian-flagged freighter discovered 11 Nigerian stowaways on board and simply threw them into the ocean off the coast of Liberia.
This is what the images of the four exhausted bodies beneath the hull of the Ken Wave conveyed— the sheer absurdity of their hiding place, the universal fears it evoked. The message was undeniable: even if you close every door, we will find a way through. Desperation is relentless. It keeps inventing new ways.
“What did I have to lose?” Thankgod says one morning shortly after his arrival—as if his own life didn’t matter.
He is sitting in the dining room of a church-run migrant shelter in São Paulo, eating a plate of rice, still amazed at where he has ended up. He knew that a few Ronaldos or Ronaldinhos played football in Brazil, but he hadn’t realized this was the same 3,000-mile route millions of his ancestors were forced to take, brought here as slaves. When he hears about it, he clicks his tongue.
“I hope they were treated well,” he says softly.
Thankgod is a small, thoughtful man in his late thirties who used to preach as a pastor in an evangelical church in Lagos. To protect himself from winter in the southern hemisphere, he wraps himself in a down jacket. As he eats, out of the corner of his eye he notices that Roman, who is wiping the tables, keeps glancing at him with suspicion.

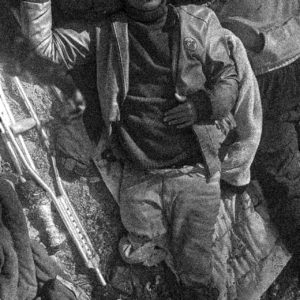
Thankgod Yeye, Photo: Ian Cheibub / DER SPIEGEL
Unlike Sunday and Destiny, who requested to be sent back to Nigeria, Thankgod and Roman were determined to try their luck in Brazil. They now sleep in a five-bed room with a Nepalese man. There are shared showers in the hallway and a room with lockers where Thankgod keeps his shampoo, a bottle of spicy sauce, and a tin of cocoa.
He is allowed to stay for three months. Every morning, he sits in a classroom with Angolans and Afghans, learning Portuguese. Staff members send him job listings or help translate during visits to government offices.
One of the priests now approaches Thankgod’s table and asks if he can stop by later to help him write his résumé.
Thankgod nods with a smile.
Once the man has left the room, Thankgod pulls out his phone and opens the photo gallery. He scrolls to the certificate of a company registration, an export licence issued by the Nigerian Export Promotion Council.
“I’m actually a businessman,” he mutters.
Tomrio World International Ltd.—the name of his company—sounded like a dream. After his geology degree led nowhere, he says, he took out a loan in 2017 and built a farm on a few hectares of red earth on the outskirts of Lagos.
Thankgod dug a fish pond. He put up a shed. He planted peanut crops and invested in machines to shell and roast the nuts and extract the oil from them. With the leftover dough-like mass, he made sweet cakes he planned to export.
“I wanted to travel,” he says—by plane, not illegally on a ship. But then, sometime last year, the rain came.
It rained throughout October.
November too.
By December, the mud had swallowed up the entire farm.
“Do you think these certificates are of any use to me here?” he asks, before swiping through the photos again.
He shows a billboard-sized church poster announcing Pastor Thankgod’s sermons. A picture of Rita, his wife, who had worked at First Bank. Their wedding photos—him in a suit and tie, her in a pure white dress. His children from a previous marriage: Cynthia and Godswill.

Rita Obiageli Yeye, Thankgods Wife, Photo: Andrew Esiebo / DER SPIEGEL

The view from Ogogoro Island onto Lagos harbour, Credit @ Andrew Esiebo / DER SPIEGEL
“We were a middle-class family,” Thankgod whispers, “but Nigeria is a country that won’t help you when you’re in trouble.”
He sees Brazil as more progressive. When he arrived and sat in the immigration office, the man explained to him that citizens in need received social assistance from the state. He was also told that doctor visits were free. These were things that convinced Thankgod to apply for a residence permit. They gave him confidence that he would soon find a job, so that he could bring Rita and the children over.
When he charges his mobile phone on the patio in the morning, his chat fills up with messages from her. Rita is pressuring him, he says. She has to hide from the creditors who are demanding repayment of the loan. When will he finally send something? So far, the only money he has managed to send is $250, donated by a newspaper reader.
This morning, he skipped language class to pick up another donation at Western Union, but the money didn’t go through. Maybe the donor misspelled his name, he tells himself. He tells Roman, who was entitled to half of this transfer, the same thing.
Roman doesn’t trust him. He thinks Thankgod pocketed the money, and is now circling him like a predator.
“Brazil,” Sunday mutters, lying on a mattress in his damp room on the other side of the Atlantic on an October morning. “I hope they’ll be happy there.”
Pale light falls on his face.
You can hear the waves crashing.
Sunday was the mastermind behind the trip. For him, only one thing counts: Europe. That’s why he’s here again, surrounded by bags of clothes, pots, and the plastic buckets where he collects rainwater to shower. As if fate, or a cruel joke of international shipping, had sent him back to square one.
The place where Sunday is now stranded is called Ogogoro, a small island in the Lagos harbor. Five hundred people live here, in modest houses or crooked shacks patched with corrugated iron. Outside, a few chickens peck at the sand. On the beach, right in front of Sunday’s door, lie the wooden boats his neighbours use to fish for their meals in the oil-polluted bay. Further along, barely 150 metres away, giant cargo ships dock at the piers—like an eternal promise against the skyline.
Sometime late last year, Sunday says, Thankgod first appeared on the island. He sometimes saw him creeping through the bushes, stashing returnable bottles in a fishing net. Roman, who had lost his job as a pipe welder during the pandemic, lived a few metres down the beach with his grandmother. Destiny, who vanished after returning from Brazil, was one of the guys Sunday used to hang out with in front of the kiosk, hoping the generator had enough diesel to charge their phones.
What connects the four of them is Ogogoro—a rough patch of earth where Nigeria’s problems collide. Around 60% of citizens live in what the National Institute of Statistics calls “multidimensional poverty”—a condition where everything is precarious: the houses, the food, the job market, which has no place for the five million students who graduate from school or university each year.
“Ogogoro is not a place you want to stay in,” says Sunday, who has been living here for three years. He had found a job over at the pier, entering ferry passengers’ names on lists for a few naira. It wasn’t what he had dreamed of. After school, he says, he wrote a novel and had a dozen copies printed at his own expense. Then he studied law for a few semesters before finding a job in a friend’s shop selling imported women’s fashion from China.
His training as a salesman was meant to last five years, but in the fourth year, a fire destroyed the boutique. It was like Thankgod’s story—one unexpected event, and everything collapsed.
“Is that it?” Sunday would ask himself, sitting on a rock at the tip of the island, watching the ships pass him by, headed for distant lands. At some point, he says, he began to study them more closely—their architecture, their logistics. He learned to decipher the coded language of the Marine Traffic app. LOS stands for Lagos. STO for Santos. Green arrows mark cargo ships. Orange for trawlers. Red tankers move under Navy escort to protect against oil pirates.

Sunday Ugbo shows, where the container ship Ken Wave was laying in Lagos harbout, Photo: Andrew Esiebo / DER SPIEGEL
“On average, they stay here for 13 days,” Sunday shouts over the wind as he steers a fishing boat toward the docks, where huge cranes unload containers from Chinese freighters. Grain carriers disappear in the dust. In front of a terminal where the food company Dangote operates a sugar refinery, he points to a ship that has just arrived from Russia.
“The Ken Wave was moored here,” he calls out.
Then he points to the mast above the bridge.
“See the radar? When it starts rotating, the engines fire up. That means the checks are over. From that moment, you have an hour to get on board.”
Sunday put his specialised knowledge to the test for the first time in 2020, but the cargo ship he hid on remained in the port of Lomé, the Togolese capital, for several days. When he ran out of food, he hammered on the hatch that connects the shaft to the engine room until someone heard him and let him out.
The following year, he tried again—and made it back to Lomé. Then came trips to Cameroon, Kenya and Angola–blind journeys, because the destinations only pop up in the Marine Traffic app once you set sail. The only time he didn’t ask to be sent back was in Algeciras, Spain—but the Spanish authorities deported him anyway, without explanation.
“Study trips,” Sunday jokes. His WhatsApp profile picture isn’t a photo but a sketch of a seedling. Next to it, a verse: The day you plant your seed is not the day you reap. Be patient and have hope.
Think big.
When Sunday sat on his meditation rock this spring, Thankgod sometimes joined him. They had started talking when Sunday went next door to buy soap and spices from Thankgod’s sister. Thankgod told him about his farm, the rain, and the debts. One day, as they watched the ships leave, he blurted out:
“Sunday,” he pleaded. “Please get me out of here!”
Sunday: When I saw that the cranes were retracing from the ship, I signalled to the others. We sat together on the beach and waited for the radar. When it started spinning, a fisherman ferried us across, paddling as silently as possible.
Roman: Then we climbed onto the rudder blade, slipped through the opening, and climbed up a ladder into the shaft. Sunday, who had been with me in Togo, had asked me to get two fishing nets. We stretched them between the walls, one on the right of the steering column, the other on the left.
Thankgod: We lay in them like hammocks. Sunday I shared a net with Destiny; I got stuck with Roman, who I had seen before in Ogogoro. It was pitch black. The water was bubbling three or four metres below us. The engines were making a hell of a noise, but we didn’t say a word.
Sunday: I opened Marine Traffic one last time. Just before we set sail, the destination flashed on the screen: Santos! Even though I knew at that moment that I would soon be back, I still felt it—a sense of freedom.
On 27 June at 7:05 p.m., the Ken Wave set sail. This 190-metre-long, 32-metre-wide ocean giant had arrived from Brazil two weeks earlier with a cargo of sugar. The return journey was an empty trip, meaning the ship was so light that the opening of the rudder shaft sat above the water surface.
Nigeria exports little apart from oil. Most cargo ships leave the country empty and depart without a load. What they do carry are stowaways.
According to a report by the International Maritime Organization, 250 young men boarded ships in Nigeria in 2017 alone. Ship insurers call Lagos a “high-risk port.”
Roman: We told ourselves that we were brothers now, that we shared everything. We had peanuts with us, biscuits, and 40 bags of water, which would last us for a fortnight. We always ate at midday, when the sun was at its peak.
Sunday: At first, I checked my Bible app once a day.
Thankgod: I prayed: Please, Lord, spare us from a storm. It’s scary enough as it is. The ship is huge, and it sways. One wrong move and you plunge down. I tried not to sleep, but I nodded off once, and when I woke up, my headwarmer was gone.
Roman: You try to lie still to protect the nets. If they tear, it’s over. Once I cut off a piece of my sleeve to replace one of the ropes we used to secure the nets to the wall.
Sunday: When we stepped on the ladders to tighten the ropes, I saw Destiny shaking. To distract him, I asked: “I wonder how Chelsea played?”
After a night in which Roman repeatedly woke Thankgod up and called him a fraud, accusing him of stealing the Western Union donation, the tension finally boils over. In the patio of their accommodation in São Paulo, his “brother” punches him in the face.
“Roman is a street kid,” Thankgod grumbles later, sitting on the pavement in front of a bakery. “I would never do something like that.”
That afternoon, he asks the fathers for separate rooms. These days, when you call him, he is often lying on the bed, head on the pillow, staring blankly into the camera. Then he writes that Rita, his wife, has been arrested. When you ask what’s going on, he answers with just one word: debt.
How much?
$8,000. Maybe more.
His blood pressure spikes so high that someone has to take him to the emergency room. Although Thankgod’s body is in Brazil, his mind is in Nigeria.
In December, after the rains, when he went to check in on his field for the first time, Thankgod simply collapsed. He lay in the mud for minutes. He took the children out of school because he could no longer afford the fees, cancelled his lease, and moved in with his sister in Ogogoro. He buried himself in the Bible under the tree in front of her house, where he read that a man who could not feed his family was not strong enough in his faith. He measured the words against his own life and saw himself not as a provider, but as someone being provided for. A failure who scavenged bottles in the bushes.
Thankgod felt ashamed.
“I was hungry and told myself it was a fasting exercise,” he says.
He searched for a way out.
In February, as Nigeria elected a new president, he put up an ad on Facebook for Peter Obi, a politician who promised more jobs and less corruption. In March, when it became clear that nothing would change, he got hold of rat poison—though there were no rats. He dismissed the idea of heading into the desert, not just because of the terrorists who hunt refugees in the Sahel for ransom, but because the transport, smugglers, and shelters cost thousands of dollars—a fortune that families often scrape together their life savings for.
A boat trip, Sunday said, costs barely ten dollars. Thankgod wrestled with himself.
As a pastor, he says, he is expected to set an example for others.
Sunday: After a few days, Destiny’s condition got worse. He had headaches, fever and started to vomit. We decided he had to eat to get his strength back.
Thankgod: I wondered what would happen if our supplies ran out. Last year, when six men from Ogogoro set out for Brazil, three returned and the others disappeared into the sea. No one knows exactly what happened in the shaft, but there were rumours of an argument, and the thought of it drove me crazy. I was afraid to sleep, afraid that I would be pushed out of the net so the food would last longer. The truth is: you are lying next to strangers, and you don’t know what’s going on in their heads.
Deep below them, at the bottom of the ocean, lay a mass grave. Five million Africans, many from present-day Nigeria, were shipped by the Portuguese to the New World from the sixteenth century onwards. Before they were chained, packed tightly in the belly of the caravels, they were baptised and branded. The mark signified that they now had an owner.
When hunger or thirst overcame them, many resorted to their own excrement.
Historians estimate that 400,000 did not survive the crossing. Those who did were funneled through the slave markets of Brazilian ports into the hinterlands, where they worked on Portuguese plantations. They planted cotton, picked coffee, or cut sugarcane—products that were transported to Europe, converted into money, and reinvested in Africa to buy more slaves.
It was this transatlantic triangular trade that first bound the continents together. It remains one of the foundations of the unequal distribution of wealth in the world today.
All that followed in Nigeria—British colonial rule, arbitrarily drawn borders that forced together hundreds of tribes and cultures into a single nation, an independence that descended into civil war, dictatorship, and a fragile state structure that differs from others in the region essentially only in that its elites are a little wealthier because of oil—all of this has never really been addressed.
In a city of millions like Lagos, not a single museum grapples with the slave trade. Only last year was history reintroduced into primary and secondary schools, after the government had removed it from the curriculum in the 1970s. At the time, Nigeria chose to look ahead. More important than forging a national identity through historical reckoning—by coming to terms with the past—was the pursuit of individual success.

Roman’s sister Julia, Photo: Andrew Esiebo / DER SPIEGEL

The view from Ogogoro Island towards the skyline of Lagos, Photo: Andrew Esiebo / DER SPIEGEL
Men like Thankgod and Sunday learn what that means from childhood. In the settlements where they grew up, the largest houses always belonged to people who didn’t live there. They heard that their owners financed their neighbors’ lives from afar. And they saw the uproar when the heroes of the diaspora came home, draped in jewelry, their suitcases stuffed with designer clothes, medicine, and toys for the children.
That only a small fraction of emigrants succeed doesn’t matter. What counts are the victory poses with which those who scrape by to afford their Western Union transfers keep spinning the legend on social media. Their success fuels the shame that someone like Thankgod feels. It raises expectations. It increases the willingness to take risks.
Today, slave hunters are no longer needed to drag people onto ships. They come on their own. Bound by invisible chains.
Thankgod: When we opened the last pack of biscuits on the tenth day, I told myself: So now the fasting begins again.
Sunday: I considered getting the hammer out of my backpack, but I hesitated. There was no harbour—it was the open sea, lawless territory. Off the coast of Liberia, a couple of men had recently been thrown overboard after hunger made them reach for the hammer.
Roman: We knocked, knocked, knocked. No one opened. The hatch was closed, welded shut, probably because of fear that pirates might board the ship. I climbed down on the rudder and looked out, but all I saw was grey. Water. Whales. Sky. I know you’re not supposed to drink salt water, but it was all I could find, except for my piss, which I once lapped up from a plastic bag.
Thankgod: When Destiny sucked the last bit out of my toothpaste tube, he vomited again.
Roman: When we boarded the ship, I was more determined than ever. Now I tasted blood bubbles in my mouth and prayed every night that the sun would rise again.
Sunday: When someone dozed off, I slapped them awake.
Thankgod: Lord, I said silently, if you get me to my destination safely, I’ll never do anything like this again.
Sunday: Thankgod was the most afraid. Once he cried when he thought of Rita. Gentleman, I said, relax! One day you’ll catch up with her.
When Rita Obiageli Yeye was released from custody in October after posting a small bail, she moved back into the house of Thankgod’s sister in Ogogoro. Days later, she is sitting on the bench under the tree where he used to read the Bible. With her colorful Sunday suit, her painted nails, and her polished English, she seems like a stranger on the island.
On her lap is a bag with Thankgod’s things: his comb, a few clothes, and the notebook where, in scrawling handwriting, he recorded the lot sizes and future yields of the farm. As she flips through the pages, tears well up in her eyes. Then she breaks down.
“What else could we have done?” she says. “Nobody lends money to people like us in Nigeria.”
When she first met Thankgod, Rita was an account manager at a branch of First Bank. People would come to the counter, hand her their money, and she would count it, recording the balance in their accounts. The temptation was always there. Every now and then, from the deposits of a wealthy man, she would slip a small bundle into her skirt.
They called it “credit” because they always planned to repay the money—once their farm was profitable.
But then, the theft was discovered. A customer filed a complaint. A legal settlement was reached, and now Rita is pinning her hopes on Thankgod finding a job in São Paulo to start paying off the debt. It’s not easy, he tells her over the phone. Jobs are scarce, and the ones he’s been offered don’t pay that well.
“Be patient,” he says. “I’m not lazy.”
Rita swallows.
“I never thought he would find the courage,” she says.
A few days after she found the rat poison in his possession, Thankgod told her he was thinking of leaving. When she asked him what he meant, he put his finger to his lips. “Trust me,” he said, “I’m doing it for us.” And then, just like that, he was gone. Unreachable. As if swallowed by the earth. Rita nearly lost her mind, convinced he had attempted to cross the desert.
Fourteen days later, she saw the images of the rescue on Al Jazeera.

Thankgod’s wife Rita in front of his sister’s house, Photo: Andrew Esiebo / DER SPIEGEL
Sunday, Rita’s neighbour, is sitting under a tree nearby during the conversation. He follows her words with an unreadable expression. Rita has never dared to ask him questions, but now she looks at him expectantly.
“Tell me,” she says, “why are you really back here?”
Sunday avoids her gaze.
He mutters something about Brazil not being for him, but everyone in Ogogoro knows that’s only part of the truth. The freighters, the others say, are a “business” for him—a “big game” in which he wins something every time.
On his “study trips,” Sunday learned that every ship has an agent who, among other things, handles the repatriation of stowaways. These agents are susceptible to blackmail because the companies don’t want any trouble. In Togo, he later said, they paid $100. In Kenya and Angola, $150. The Brazilian agent of the Ken Wave offered him $2,500 just to avoid extra costs for the shipping company, which had to pay for the repatriation.
Sunday grinned.
It was the best-paying job of his life. In 14 days, he made as much as he had in three years at the port desk.
With the money, he paid next year’s rent, invested in his sister’s hairdressing salon. He had also struck a deal with Thankgod. He won’t say how much he charges for his smuggler service, but he knows one thing—you don’t harvest the fruit on the day you plant the seed.
While the boys in Ogogoro pressure Sunday to get them on a ship, Thankgod has become the first in his family to hold the identity document of a foreign country. Now, he is searching for a place to stay in São Paulo. The priests told him it was time to stand on his own two feet.
On a sunny October morning, he is sitting on the patio. He says he didn’t have to think about it for long—his problem is bigger than $2,500. Rita is breathing down his neck about the debt. Sunday is demanding the $100 they agreed on. His sister reminds him daily that his nephew’s birthday is coming up.

Sunday studying one of the ship apps that he has used to acquire specialised knowledge, Photo: Andrew Esiebo / DER SPIEGEL
It’s a flood of messages.
Everyone wants something from him.
At night, he sometimes pushes a wheelbarrow through the market. During the day, he washes dishes in a restaurant.
“I need something real now,” he says, scrolling through job listings.
A plantation that grows pine trees and sells bark extract to perfume manufacturers is hiring unskilled workers. They offer minimum wage plus food, accommodation, and transport. It doesn’t sound so different from 135 years ago when Brazil became the last country in the Americas to abolish slavery. The only difference is that now, there’s free WiFi.
Thankgod hesitates.
“Three hundred dollars isn’t much,” he says. But it’s what Brazil has to offer someone like him. The country is more open than Europe, but the modern low-wage slaves are still left with almost nothing.
Thankgod, Roman, Sunday, and Destiny were brothers for 14 days after the Ken Wave departed from Lagos—a community bound by fate. Today, they are each going their own way. Roman now spends more time with a Ghanaian who arrived recently on a container ship. Sunday will probably try again soon, once his money runs out. Destiny is still nowhere to be found.
As for Thankgod, he has done the math—it will take years before he can afford a plane ticket for Rita.
He runs his fingers over the comb she had slipped into one of his books back in Ogogoro, asking him to bring it with him.
Sometimes, he says, he thinks about breaking up with her.
To finally move forward.
Further Credits:
- Julia Prosinger, editor at Der Spiegel
- Ian Cheibub, who took the pictures in Brazil
- Andrew Esiebo, who took the pictures in Nigeria
- Dan Ikpoyi, who worked as a fixer in Lagos
“Because if I Die, No One Will Care.” Children’s Day at the Border
Is that her? I was supposed to meet a teenager, but in walks a slightly hunched young woman. Petite, about five feet tall, with long, bleached hair. Henna-tinted eyebrows and full lips.
We sit in the kitchen of an old wooden house, now home to new residents. They wanted to escape the city. When refugees started appearing in the forest, they took to helping them.
“Hila, have you eaten?” Maria asks.
“No.”
“What do you want? An egg? Egg [in English in the text, translator’s note]?”
“Yes.”
A puppy nibbles at our ankles. A monitor displays the driveway outside. When Maria and her husband started going into the forest, they installed cameras—law enforcement agents shine lights into their yard and note down car license plates.
We head to Hila’s room. She sits beneath a wall covered in religious icons. Among the collection of Pope John Paul II’s portraits, she has stuck notes in Farsi reminding herself not to eat sweets—they make her stomach hurt.
“What is it like to be here?” I ask Hila.
“Like a dream. In Afghanistan, I saw places like this only in movies.” Hila speaks softly and slowly, repeatedly buttoning and unbuttoning the cuff of her checkered shirt. Her eyes glaze over only once—when she recalls the moment in the forest when she felt utterly unwanted.
“Hila” means “dream” in Farsi. That’s the name she chose for this report, though for now, she lives without dreams.
I wanted to be a doctor
Before she lost her dreams, Hila lived with her mother and sisters in a house with a garden. She never met her father—a high-ranking policeman killed by the Taliban before she was born. Over time, her older sisters moved out, and her mother remarried. Her stepfather did not work. He slept, smoked hashish, or went out. He sold things from the house to buy drugs. Never food for them.
“My younger sister and I were hungry,” Hila admits. “And my stepfather was always yelling at me. I didn’t know he wasn’t my real father. The neighbours told me when I was nine.”
Hila’s mother worked as a cleaner and cook so they could eat. At 14, she was married off early, had daughters young, and always told them: Study. One of Hila’s sisters became a gynaecologist and stayed in Afghanistan with her husband. The other graduated from university and moved to the U.S.
Hila studied hard, too. “I dreamed of becoming a doctor like my sister. I loved her white coats. Sometimes she dressed me in them and took me to the clinic,” she says, smiling.
Four years ago, their mother died of stomach cancer. “She was 53,” Hila whispers. “She always told us we must be free, strong, and independent.”
My stepfather sold me
Six months later, the Taliban took over. Hila was 16 years old. One day, her stepfather announced that he was taking her younger sister to visit his family, and Hila was to stay behind.
Cars pulled up in front of the house. Strangers came in, saying they were taking Hila to her father and sister, but they took her to a building where they were nowhere to be found. “He sold you,“ she was told. The man who had “bought” her claimed to be her husband. He imprisoned, beat, and raped her.
She managed to escape. In Kabul, she bought a fake passport and a student visa to Russia. Her half-sister, whose husband worked for the Germans, helped. Before the Taliban arrived, they were evacuated to Berlin.
Hila wanted to get out of Afghanistan.
At the airport, the guards asked where she was flying to. From under her hijab she whispered that she was joining her husband and would study in Russia. They said she should study in Afghanistan. “But girls can’t,” she thought, but only repeated that her husband was waiting in the Emirates. They let her board the flight—through Dubai to Moscow.
After a year, her visa expired. Everywhere she went, she was told it could only be renewed in Afghanistan.
Luckily, she met an Afghan family planning to go to Germany with their young child. She joined them.
The men dug a tunnel
Hila tells me how she arrived at the Polish-Belarusian border.
They were stuck in Minsk for two months. Hila shared a room with an Afghan woman and her child, while up to 20 men crowded into another. The Afghan family was short on money and was looking for a cheap smuggler.
People who had returned from the border would visit their apartment. They spoke of being bitten by dogs, running out of food, or being beaten. But some later called from Germany.
At the end of May 2023, Hila and the entire group arrived at the Belarusian border. The men dug a tunnel.
“You had to squeeze through headfirst and reach out your hands, while someone on the other side pulled you through,” Hila recounts. “I didn’t worry about whether it was legal because everyone did it. Pregnant women, the elderly, small children.”
Then they fell asleep in the forest.
He was playing with a cat, yelling at people
“When I opened my eyes, I saw a big dog and Belarusian guards. I covered myself with my hijab and kept repeating: ‘I can’t see you.’”
They beat one of the men and packed everyone into cars.
“I prayed that they would not send us deep into Belarus. We had already spent seven days in the jungle. Soaking wet, without water or food.”
At night the Belarusians drove them somewhere. There were already 150 people there, and the guards kept bringing in more.
“They beat the Africans very badly,” Hila shudders. “I noticed a family with daughters. One of them was holding a cat. A guard smiled and played with the cat. At the same time, he yelled at people and shoved them. That’s when I realized this wasn’t a movie. This was my life.”
The Belarusians drove them to the middle of the forest. They picked a leader, left him with a phone and a power bank. They took the rest. Then they said:
“Go. If you come back, we will beat you. Or kill you.”
Hila knew some Russian. She translated the message to the rest of the group.
They walked for days again. It rained nonstop. Hila was drenched, unable to remove the insects tangled in her hair. Her head and face swelled, red from bites, while her feet turned white from the water in her shoes. She was freezing.
“There was a 13-year-old boy with us, all alone,” recalls Hila. “He looked at me sadly.”
He tried to get up but got dizzy and collapsed.
Someone in the group muttered that he hadn’t eaten or drunk anything for a long time. We drank water from the leaves and from the ground. I don’t know how many days I spent in the jungle [sic, translator’s note]—I think two weeks.
Nobody needs me
By mid-June, they reached the Polish border. The men decided to make a ladder. They set fire to a tree and burned it until it could be broken. It took them two days. They tied the rungs with shoelaces. In the evening, they went to the fence. Hila climbed the ladder. She doesn’t know how she fell on the other side.
When she opened her eyes, she saw three unfamiliar boys. They handed her an energy drink.
“I will never forget that lemon taste,” Hila smiles. “They were also from Afghanistan. They said that after me, many more people went over the fence, and no one stopped. I lay like that for several hours.”
One of the boys carried her on his back. He was thin and not very strong, so he left Hila’s backpack with all her belongings behind. When he tried to put her down, she couldn’t stand, not even for a moment. Another one took her on his back.
In the morning, she told them: “Leave me, go. If the police found you, I’d feel guilty.” But they kept repeating: “No. If we get caught, we’ll cross again.”
They made a makeshift stretcher and kept walking. They tried to make her laugh, kept her awake. They climbed trees to find signal and call for help.
They called out: “Help! Help!” No one answered. Using perfume, they lit a fire. One shouted:
“I’ll burn this whole fucking jungle! Why is no one here?!”
They carried Hila closer to the fence. One stayed behind while the others went to get help.
“When they came back, one of them sat down and started crying. I asked why. And he said: “Why aren’t you crying, why aren’t you screaming, why aren’t you sad?”
I told him: “Because if I die, no one will care. Nobody needs me.”

Photo: Agnieszka Rodowicz

Photo: Agnieszka Rodowicz

Children behind the border fence. May 2024. Photo by Agnieszka Rodowicz.
I was full of ticks
Eventually, the activists came. The boys were given food, dry clothes, and shoes. One gave Hila $200, and they moved on. The medic gave Hila a painkiller and called the state ambulance.
“The way to the ambulance was terrible,” Hila recalls. “My legs kept hitting trees and bushes. Every touch caused excruciating pain. In the ambulance, I started screaming because the pain was getting worse. The paramedics yelled, ‘Shut up!’ while I wailed and sobbed all the way to the hospital.”
Hila sent a message to her stepsister. “If it wasn’t for her, I wouldn’t be here. I have to repay her for everything she did for me,” Hila’s voice trembles.
They sent her to another hospital, where they finally removed her wet and dirty clothes. She was full of ticks.
I have six metal implants in my back
When she opened her eyes, she had four IVs, and a large machine was pumping painkillers into her. Despite this, she cried from the pain.
After two months, her arms were covered in wounds from the IVs. She couldn’t move, wash herself, or do anything on her own. She asked the nurses to cut her hair. They protested. Instead, they fed her, made her laugh, and gently washed her head—then, piece by piece, her entire body.
“It was an amazing feeling after two months without washing!” she recalls.
After weeks of rehabilitation, with the help of the nurses, she managed to sit up.
“I was so happy to see my feet! The physiotherapists asked me to move my leg. I couldn’t. I was terrified they would amputate it.”
By the middle of the third month, Hila received crutches. The nerves in her operated leg were damaged, so she couldn’t feel pain. As soon as she managed to stand, she started walking. First with two crutches, then one, then eventually on her own.
“I have two screws in my foot, six metal implants in my back. To this day, I have no sensation in certain parts of my body. They said it should improve after another surgery. Maybe.”
Anatomy atlases of the white race
When undocumented foreigners claim to be minors, the Border Guard refers them for an age check. They take an X-ray of their wrist or assess their teeth.
“There is no method that can confirm a person’s age with 100% accuracy,” says lawyer Ewa Ostaszewska-Żuk from the Helsinki Foundation for Human Rights. “The margin of error in these tests is two years. On top of that, they rely on so-called anatomy atlases from the 1950s, based on studies of the white race. These are not applicable to people from African or Middle Eastern countries. Yet doctors don’t take that into account.”
“For Europe, determining age, the calendar—it’s a fetish,” adds Maria. “In many countries, kids don’t even know their exact birthdate. And really, what difference does it make whether someone is 17 or 19? Everyone deserves decent treatment.”
“Sometimes people have two documents with different birthdates,” adds Jarek. He and his wife Asia care for unaccompanied teenagers in hospitals and support them when they move into foster care.
“Some people don’t know how to write their birthdate in the Anglo-Saxon format—or at all—because they are illiterate,” says Jarek.
“There are countries where the calendar is completely different, adds Asia.
“We are caring for someone from Afghanistan who was born in the year 1375. Higher mathematics is needed to convert that.”
The Border Guard had no doubts about Hila’s age because her sister sent a copy of her identity document. Even so, it took a long time to find a care facility for her—there simply weren’t enough places.
“As a result, the Border Guard delays accepting applications from underage foreigners,” explains Agnieszka Matejczuk, a lawyer from the Association for Legal Intervention (SiP).
Not enough places, a makeshift guardian
According to the law, a foreigner aged 15 or older who is undergoing return proceedings leading to deportation may be placed in a Guarded Center for Foreigners (SOC). However, if they are under 15 or apply for international protection, they cannot be detained there. The application, however, must be submitted in the presence of a guardian. The minor can declare their intent to seek protection, which obligates the Border Guard (SG) to transfer them to a care facility and request a guardian.
“But there are not enough places in care facilities, nor are there enough guardians, so the SG often ‘doesn’t hear’ minors’ declarations,” adds Matejczuk. “We are one of the few EU countries where there are no professionals trained to act as guardians. There is also no single person responsible for safeguarding the child’s interests. The court appoints a guardian for each case. By law, it has three days to do so, but in practice, this can take up to five weeks.”
A candidate for the guardian role should be a legal adviser, an attorney, or a representative of an NGO providing legal aid to foreigners.
“But no one volunteers, so the court picks someone at random, often someone without the necessary knowledge,” says Olga Hilik from SiP.
Care facilities are also reluctant to accept refugee minors.
“They explain that there are not enough places,” says Hilik. ”However, they are legally obligated to accept a child when the SG brings them in. Still, it is common for a child to be sent away.”
For a young person, it is crushing to feel like no one wants them.
This creates a massive systemic gap.
Did I break my back for this?
Hila applied for international protection in Poland but wanted to join her sister in Germany. The family reunification procedure can apply to siblings, but the fact that they were half-sisters complicated matters.
Hila, who at the time was still unable to walk, was supposed to be placed in a care facility for people with disabilities. When a place was finally found, the court ruled that a child could not be placed there without a disability certificate. But such a certificate cannot be issued to someone in asylum proceedings.
In the end, a place was found for Hila in a children’s home. The director claims that the Border Guard never consulted her. They simply stated that Hila would be staying there and that was that.
“I was supposed to share a room with another girl. She didn’t want to be with me,” Hila recalls. “Little kids would come up to me and ask, ‘Where are you from? Show us your country on the map.’ The older ones weren’t so nice. I thought: Is this the life I came here for? Did I break my back for this?”
“A few days later, she went with the other orphans to Jasna Góra,” says Maria. “Children’s homes in Poland are very church-oriented. This is a problem because not all the kids there are Christian. Hila isn’t.”
“When I was in pain, when I was sick, I asked for medicine, for painkillers, but the caregivers told me they couldn’t give me anything,” Hila says. “For the other children, they had plenty of medicine. They gave them vitamins, but not me.”
Sometimes, the home would order McDonald’s for all the children—except Hila.
“Is there anything you like in Poland?” I ask her.
“Karolina.”
Karolina, a social work educator specializing in rehabilitation, previously worked with children with autism. For the past two years, she has been supporting minors who arrived in Poland via the Belarusian border. Like Maria, she works for a foundation in Podlasie. They do not disclose its name or their full names, as they don’t want to worsen their already difficult relations with children’s homes.
“I act as a kind of intermediary,” Karolina says. “I connect psychotraumatologists with care facilities, doctors with guardians, lawyers with children.”
I painted a blonde woman in flames
We take a walk around Maria’s house. In the yard are chickens and ducks. “Happy Woman’s Day,” Hila says to them, because it happens to be 8 March. She talks about how Karolina would pick her up every few days from the children’s home and take her to rehabilitation. Karolina also invited Hila to her home for Christmas.
After four months, I was finally in a real home,” the Afghan girl recalls. “We sang, we cooked. I also went to the cinema for the first time in my life. It was wonderful. I felt like I was in a film.”
Karolina brought her a sketchbook and paints. Hila painted a field of flowers, coils of razor wire, and a blonde woman in flames. Since then, she has painted dozens of pictures.
And what does Hila’s future look like?
“They are going to put a prosthesis in my spine. Maybe then I’ll regain feeling. I’d like to go to school.”
We go back to Hila’s room.
“I think the worst is behind me, but things aren’t great,” she says. “When I have a problem, I say: ‘Gods, help me.’” She laughs, pointing to the holy pictures on the walls. There’s also a clock with an invocation to Allah and a prayer from the Quran embroidered on a tapestry.
“I still believe there is someone up there.”
“What else keeps you going?”
“That I have a younger sister. I will do anything for her. For now, I don’t know where she is. I hope she is alive and that my older sister will find her.”
If a child speaks Pashto
Two years ago, two teenage girls from African countries were caught by the Border Guard. They were placed in a children’s home in Podlasie. They spoke only French and could not communicate with anyone. For six months, no one issued them a PESEL number or any documents, so they could not attend school. They complained about being left to fend for themselves. One of them had a toothache for two weeks, but the caretakers only gave her painkillers. Looking for help, they found Karolina’s foundation.
“When I first dealt with children’s homes, I took certain things for granted,” Karolina admits. “I assumed that the home would provide medical care and education. It turned out that wasn’t the case. We arranged online Polish lessons for the girls and made a dentist appointment. A complex root canal treatment was needed,” Karolina explains.
The activists also found the girls a French-speaking psychologist. They took them for walks and shopping.
“Children from the border have nothing, sometimes not even a comb, let alone winter boots,” says Karolina. “We help because the facilities lack resources and staff. Some children’s homes do what is legally required, others put more heart into it. Some don’t even try to find a translator, yet the children sometimes speak only Pashto, Dari, or Somali. So, we look for translators, either in person or by phone.”
The African girls had stomach problems—they were not used to eating white bread twice a day. The activists bought them beef, semolina, and vegetables so they could cook for themselves. The children’s home accused the women of spoiling them.
“I feel like some facilities are just waiting for these children to run away, for someone to take them,” Karolina says. “And they do disappear. Most often boys, but girls too. Not knowing the country or the system, they can easily fall prey to traffickers.”
Director: The girl should give birth
Usually 16, 17-year-old girls don’t talk about it.
“They are ashamed and afraid. In their countries, raped women can be sentenced to death,” Karolina explains. “Besides, after training with La Strada, we know that people who have gone through such experiences, even when they are under care, think it’s just another stop on a trafficking route. We don’t know the full scale of it because women rarely speak about it.”
“We are convinced that there are no women at the Polish-Belarusian border who have not been victims of sexual violence,” adds Maria. “In their home countries, in Russia and Belarus, and at the border itself. From what we hear, also at the hands of Polish services. If we suspect something, we should report it to the authorities. But calling them in the forest could result in deportation, exposing the women to more rape. That’s why we don’t call them.”
One of the African girls arrived in Poland pregnant, the result of rape in Russia or Belarus. She did not want to give birth. A lawyer filed a request with the court for permission to terminate the pregnancy. The children’s home was against it. The director stated outright that the girl should give birth. However, the court ruled in her favour, and the pregnancy was terminated in a hospital.
“Our charge was treated with great compassion and understanding there,” Karolina recalls.
Border children left on their own
“We believe that trafficking victims should be as far from the Belarusian border as possible,” Karolina says.
La Strada helped relocate the girls to Warsaw.
“Our contact with the capital’s children’s home showed that everything can be arranged with a little effort. We were invited to meetings. We shared information about the girls because they trusted us and stayed in touch.”
Unfortunately, one of the girls disappeared. She was not yet of age.
“We don’t know if traffickers took her—there is that risk,” Karolina says. “Border children left on their own can get into trouble. Fortunately, if they are studying, they don’t have to leave the children’s home after turning 18. If they had to become independent in Poland after just a year or two, it would be very difficult,” she adds.
Knowing that one of the girls dreamed of becoming a model, the activists arranged a real photo shoot for her. It turned out she had talent. Unfortunately, the Office for Foreigners (UDsC) did not issue her any documents or work permits for a year and a half.
Help in the forest is a piece of cake
Medical knowledge in care facilities is also poor.
Since 2015, Petra Medica has been implementing an agreement with the Office for Foreigners (UDsC), providing medical care for foreigners, including minors applying for protection in Poland.
“But Petra Medica, just like the National Health Fund (NFZ), is reluctant to issue prescriptions, and treatment is not immediate,” complains Karolina. “Hila can’t wait, so we look for treatment privately.”
The Foundation also arranges for the girl to be seen by a traumatologist.
Refugee children who are in foster care do not receive any money from the state.
“The issue of the 800+ program is unresolved. One lawyer said these children are entitled to it, another said they are not,” complains Maria.
Foster homes provide actual care but do not have the authority to make decisions regarding medical matters. Even anaesthesia for dental treatment or rehabilitation requires consent. When a hospital sets a surgery date, a court decision must be made in time to approve it. Previously, before the consent came, Hila’s broken heel healed incorrectly.
“Obtaining legal custody of a child is complicated. In Hila’s case, we would need to prove, for example, that her parents are deceased,” says Maria. “How, when Afghanistan does not issue death certificates? The help we provide in the forest, including wading through swamps and hiding in ditches from the Border Guard, is a piece of cake compared to helping these children. It’s black magic and bouncing from door to door.”
“Schools require documents confirming where the children have studied,” adds Karolina. “There is no way to get them from their countries of origin, so finding a school in Poland is a miracle. The authorities have changed, and we have reported all the problems to the Ombudsman for Children. Maybe something will be done about it,” the activists hope.

A POPH activist monitors the situation of people gathering at the Polish fence, especially a group of underage Somali girls. Photo by Agnieszka Rodowicz.

Photo: Agnieszka Rodowicz

A volunteer from the Ocalenie Foundation visits a lonely teenager in the hospital, who was found in a Polish forest near the border with Belarus. Photo by Agnieszka Rodowicz
The doll sings about freedom
When we meet again, Hila is wearing a thin ecru blouse, which emphasizes her porcelain complexion. She has sharp black nails with white patterns. She has something of a businesswoman about her. She jokes with Maria that she would manage the foundation’s money better. The Afghan girl is staying at Maria’s house.
“She sees the foster home as another prison. We managed to arrange things, and the facility allowed Hila to take a leave. The girl was revived,” says Maria.
I ask how the village has reacted to Hila’s presence.
“We don’t talk to the neighbours since they found out we were helping in the forest,’” says Maria.
Hila takes a big mermaid doll out of a box, presses her tummy, and the doll sings.
“She sings about freedom,” explains Maria. “We found it in the forest, like many other things belonging to the refugees.”
Hila hugs the doll and browses through some documents, a receipt from a jeweller, banknotes, and a Bible in Arabic.
“I had perfume with me that my mother used and a tiny prayer book I got at the mosque. Everything was lost in the jungle. I lost my phone, documents, and dreams there.”
Lone teenagers wander in the wilderness
From 1 July 2021 to 31 December 2021, the Border Guard recorded eleven unaccompanied minors on the Polish-Belarusian border.
Colonel Andrzej Juźwiak, acting Spokesperson for the Commander-in-Chief of the Border Guard, claims that for 2022-2023, there is no such data. The Wearemonitoring association, which monitors the humanitarian crisis at the border, registered reports from 139 minors without guardians in 2023.
Since mid-March, activists have reported an increasing number of lone teenagers wandering in the Bialowieza Forest. From the beginning of the year to the end of April, the Border Group has already received 134 reports from them. Many have no plan, leading to so-called “revelations” to the Border Guard.
“If there are witnesses, most protection requests are accepted,” says Michał, an activist from the Border Group. “The Border Guard in Dubicze Cerkiewne and Bialowieza is overwhelmed and sends ‘clients’ to other facilities in Podlasie, which are not prepared for it. If there are no witnesses to the detention, refugees are pushed back to Belarus, regardless of age or whether they want protection or not,” Michał claims.
Pushbacks from Border Guard facilities and hospitals still occur. Wearemonitoring is aware of at least 28 minors being pushed back from the beginning of the year until the end of April.
On 27 May 2024, Andrzej Juźwiak responded: “This year, no unaccompanied minor has been recorded at the border section with Belarus.” He also claims that the Border Guard is in contact with care facilities, and there are available places there.
Huge groups of minors are coming
According to activists, orphanages are packed to the brim. Olga Hilik from SiP says that even intervention centres no longer want to accept minors. Perhaps that’s why, when the Border Guard takes people claiming to be minors for age testing, most “turn out” to be adults.
Juźwiak claims that from January 1 to May 20, 2024, only 9 unaccompanied minors were admitted to SOCs (closed camps for asylum seekers), and currently, there is only one there.
Olga Hilik says that in Przemyśl alone, there were six minors recently.
“Because huge groups of minors aged 16-17 are coming,” says Asia. “Mostly Somali teenagers, the majority of which are girls. We ask them if they knew each other before embarking on the journey. No. They read on Facebook that it’s enough to get to the fence and they’ll be let in. Their brother or sister, already in Belgium or the UK, sends money, and the kids go.
If they get through the fence, some end up in orphanages, some in SOCs or open centres. And most of them first go to the hospital. With stomach problems from drinking swamp water, respiratory and urinary infections, hypothermia, exhaustion. There are also broken limbs, torn knee ligaments, and cuts from the barbed wire.
“But above all, they are terribly dehydrated and malnourished,” says Asia. “Especially those who survived the winter in Belarus. They look like they’ve just come out of a concentration camp in Auschwitz.”
Crawling through the Bialowieza Forest
At the end of March, several aid groups received a call and photos of a young Yemeni man. He has no right leg, the other is partially disabled, and he complains of kidney pain. He tried to walk on crutches but couldn’t manage, so he crawled through the Bialowieza Forest. For two months, I asked activists from different groups if they knew what happened to him. They didn’t know.
Since the beginning of April, the Podlaskie Voluntary Humanitarian Rescue (POPH) has been in contact with a lone 16-year-old from Egypt who asked for help. Around April 20, activists received another call from him. Polish soldiers caught him in the forest. He showed them a request written in Polish on his phone: “I am a minor. Please grant me international protection in Poland.” They smashed his phone and threw the boy back into Belarus.
”We went to the fence to see the boy and make contact with him,” says Agata Kluczewska from POPH and the Free Us Foundation. “He spent two years in Belarus, was on the Latvian border, and endured torture there. We reported the case to the Border Guard, the police, the Ombudsman, and the Children’s Rights Ombudsman. We wrote to family courts and the European Court of Human Rights.
“We don’t know what, but something worked,” says Agata Kluczewska.
The boy was allowed into Poland. Information about the action spread on the internet. Since then, POPH has been receiving more calls for help every day.
For a month, activists have been monitoring the situation at the fence almost 24 hours per day. They report that soldiers and Territorial Defence troops calmly eat in front of starving people. They walk along the fence listening to loud disco-polo music on their phones.
However, it also happens that Border Guard patrols, at the request of activists, pass food, sleeping bags, and clothing to people on the other side of the fence.
“But often, we hear from the military: ‘No one was here today,’” says Kasia Mazurkiewicz-Bylok from POPH. “And from behind the fence, we get a photo of a soldier facing the person taking the picture. Or a message: ‘They sprayed us with gas, we ran away.’ At the end of May, even a baby was sprayed with gas.”
How the hellish lottery works
When people gather by the border post, POPH collects their details—shouted through the fence, or sent by phone. And dozens, hundreds of photos of injuries. People complain of stomach pain, asthma, breathing problems, allergies. There are people with heart attacks, broken spines, partially paralyzed, bitten by dogs, stung by insects so badly they can’t open their eyes, unconscious. Pregnant women, those who have miscarried, cancer patients, people with festering wounds, burns, vomiting children.
Activists write emails wherever they can and get no response. Ten, twenty, fifty times.
“We keep writing, calling, because sometimes it works. Maybe, because someone gets let in or taken away by ambulance,” says Agata Kluczewska. “We put more people on the list. Often, three are let in. We don’t know why those three. We don’t know how this hellish lottery works.”
A call and photos of a young Yemeni man came to aid groups. He has no right leg, the other one is disabled. He tried to walk on crutches. He couldn’t, he crawled through the Białowieża Forest. For two months I asked activists if they knew what had happened to him. Photo. Agnieszka Rodowicz.
Girls desperately cling to the fence
On a weekend in May, I join the activists at the fence. I find a boy from Yemen behind it, missing a leg. He sits on the Belarusian side, but on Polish soil. He smiles shyly and places his hand on his heart. He was fleeing the war. He probably stepped on a landmine. He sends me a photo. His leg is amputated high above the knee. Next to the boy, there are crutches. Just beside him sit several girls, and teenage boys are milling around. At night, the Belarusians come back, hunting people. The girls scream desperately, clinging tightly to the polish fence. The Belarusians drag them away, tossing food and sleeping bags into the fire. A red column of flame bursts out.
In the morning, people return to the fence. Families with children, young and old men, middle-aged women. And lone teenagers. From Somalia, Eritrea, Ethiopia, Syria, Yemen.
Raped girls, boys beaten by Polish and Belarusian services.
Exhausted, Abdullahi leans against a fence after a pushback.
Fatima, with diabetes, has no medication.
Zeinab complains of stomach pain.
Brothers Adam and Khadir, ask for water and food. They stretch their hands through the fence.
The soldiers do not react. Between Poland and Belarus, a tricolour cat strolls by. We can feed her, but not the children.
Further Credits:
Włodek Nowak – editor
The report was made possible in part thanks to the support of the Foundation for Polish-German Cooperation (FWPN).

